Ho, Ho, Ho, Uh oh! Winter Holiday Hazards
Regardless of how you spend the winter holiday season, there is much fun to be had for people and their pets!
I have always spent this season surrounded by food and family and it was not until I studied for and became an RVT that I
realized how treacherous this season can be.
There are toxins a plenty out and about during this time that pets can get access to. It can make for a most wild ‘sleigh ride’ at local general veterinary practices and emergency facilities.
As veterinary professionals, we need to have a good understanding of what toxins are problematic and what diagnostic tools are needed to help us understand our patient’s status.
Common Holiday Toxins
There are multiple toxins that we can expect to see during this time of year. We are going to quickly review some of the more ‘common suspects.’
Chocolate

Chocolate ingestion is very common most times of the year but exposure to it is much more common during the winter holiday season. A lot of chocolate products are wrapped and put under holiday trees, in stockings, and left out in bowls as treats. Curious dogs often cannot resist having a little taste!
Chocolate, as we know it, is derived from the roasted seeds of Theobroma cacao. The primary toxic substances in chocolate are methylxanthines (specifically caffeine and theobromine). These substances are in greater concentrations in darker chocolate, the least amounts are in white chocolate.
Side effects of chocolate ingestion typically occur 6-12 hours after ingestion and in the early stages can include vomiting and diarrhea, increased thirst, increased urination, restlessness, or lethargy. Without intervention these clinical signs can advance to hyperactivity, ataxia, tremors, rigidity, and seizures. In the worst cases life threatening tachycardia and premature ventricular contractions can occur.
This toxicity is typically seen in dogs but do not rule out our feline friends. Even though cats do not typically go after chocolate as readily as dogs, there are some out there that quite like it (one of my own included).
Treatment for chocolate ingestion needs to be timely and should include the following, emesis, activated charcoal, cardiovascular monitoring, management of tremors/seizures if occurring, supportive care, and fluid diuresis.
Caffeine can be reabsorbed by the bladder wall, increasing the time of clinical signs. Make sure to keep the patient’s bladder empty with urinary catheterization or frequent trips outside.
Poinsettias and Mistletoe
Poinsettias are a beautiful plant with a bad reputation!

FACT: Poinsettias are NOT toxic! If a cat chews on them, they contain a milky sap that can irritate the mouth. I would not like a cat to chew on them, but it will not harm them severely if they do. You do have to make sure clients are mindful that the cat has not stopped eating because of the temporary mouth irritation.
Mistletoe is a slightly different story depending on the variety of mistletoe (American versus European). The most common European types are Viscum album and Viscum cruciatum. The Viscum album has small white and yellow berries versus the Viscum cruciatum which has small red berries. The most common mistletoe seen in North America is Phoradendron leucarpum, or American Mistletoe. It has clusters of larger, white berries. European Mistletoe is more toxic than American Mistletoe. Toxicity is caused by the lectin, viscumin. It is a cytotoxin.
In mild ingestion cases, symptoms can be self limiting and generally include gastrointestinal irritation signs (drooling, vomiting, abdominal pain, etc). In more significant ingestions you could see collapse, abnormal heart rates, ataxia, hypotension, and even seizures and death have been reported.
Like chocolate toxicity, the treatment for this should be timely including decontamination with emesis, activated charcoal, IV fluid support, cardiac monitoring (depending on severity), and potentially hepatoprotective medications.
Prognosis for this ingestion is good with proper intervention. With more severe toxicities, veterinarians may want regular monitoring of liver values for some time after initial treatment.
Antifreeze Poisoning
 Antifreeze poisoning is a toxicity that strikes fear into the hearts of most veterinarians and technicians. Fortunately, with changes in vehicles over the years and better client education, I have seen this toxicity less frequently as time has gone by.
Antifreeze poisoning is a toxicity that strikes fear into the hearts of most veterinarians and technicians. Fortunately, with changes in vehicles over the years and better client education, I have seen this toxicity less frequently as time has gone by.
The active ingredient in antifreeze is ethylene glycol or methanol. It is, unfortunately, suspected to be very sweet and palatable and many dogs and cats can be attracted to it.
This is a complex toxicity. Very briefly, when this toxin is ingested, it is metabolized. The by-product of the metabolism of ethylene glycol causes irreparable kidney damage and failure.
This toxicity presents is three stages typically. They are briefly outlined as follows:
Stage 1 (30 minutes to 12 hours post ingestion) – central nervous system signs are seen here, almost as if the animal is intoxicated. Expect to see ataxia, depression, difficulty getting up, potentially vomiting, and PU/PD.
Stage 2 (12 – 24 hours post ingestion) – this, in my opinion, makes this toxicity so much worse. In this timeframe the animal may appear to improve, even be normal. During this time the ethylene glycol is being metabolized to the dangerous by-products mentioned above. Damage, and irreparable damage, is happening during this time despite the animal seeming better.
Stage 3 (36 – 72 hours post ingestion) – the toxic by-products have built up to dangerous levels resulting in acute renal failure, seizure, coma, and death.
Very little antifreeze is lethal in dogs and cats. As little as 0.5 teaspoons per pound is lethal in dogs, and cats only need to drink 1 teaspoon total.
Intervention needs to be immediate and aggressive. If treatment does not happen in 5 hours or less post ingestion, the prognosis is guarded to poor. If signs of renal have started, the prognosis is poor.
Emesis is not successful with this toxin due to its rapid absorption and therefore treatment is centered on the prevention of the toxin from metabolizing to its more toxic forms.
Antifreeze toxicity is important to discuss with clients during the winter and holiday time. Ethylene glycol can still be found in a variety of places such as, older vehicles, windshield de-icing agents, snow globes, winterized toilets, brake fluid, and some motor oils. This is not a conclusive list.
Onions

Onions are pervasive through most cooking so they will be even that much more abundant during the holiday season. Onions are part of the Allium family, all things in the Allium family are toxic. This family encompasses all the following: garlic, leeks, shallots, chives, and onion powder.
All members of the Allium family can cause damage to RBC’s and can cause anemia in both dogs and cats.
Signs of onion toxicosis can include hemolytic anemia, hemoglobinuria, vomiting, weakness, and poor pallor.
Treatment generally consists of emesis, activated charcoal, and supportive care as needed. These patients need to be monitored for hemolysis, azotemia, and decreased PCV. Prognosis is typically good.
This is an important toxin to remind clients of because all too frequently dogs (and some cats) get dressing that has onion or pieces of turkey that can have onion powder. It is a very easy toxicity to have happen.
Macadamia Nuts

Bowls of mixed nuts can be found any time of year, but they tend to be more readily available during the holiday season. Curious dogs often cannot resist using them as a chew toy and cats have been known to knock them out of bowls and play with them (giving dogs even easier access to them). The larger, shelled nuts often make irresistible toys to chase around hardwood floors.
Despite the cats sometimes enjoying playing with the nuts, the toxicity is seen in the dogs. Ingestion of 2.4 grams/kg of macadamia nuts can cause toxicity symptoms. How this toxicity works is not known at this time.
Approximately 12 hours after ingestion these dogs can exhibit tremors (and related hyperthermia), ataxia, general weakness, vomiting, and depression.
Treatment is typically centered on removing what can be removed by emesis and then slowing absorption with activated charcoal. Most dogs do not need anything more than that however, if the clinical signs are significant, hospitalization and supportive care may be required.
Diagnostic Testing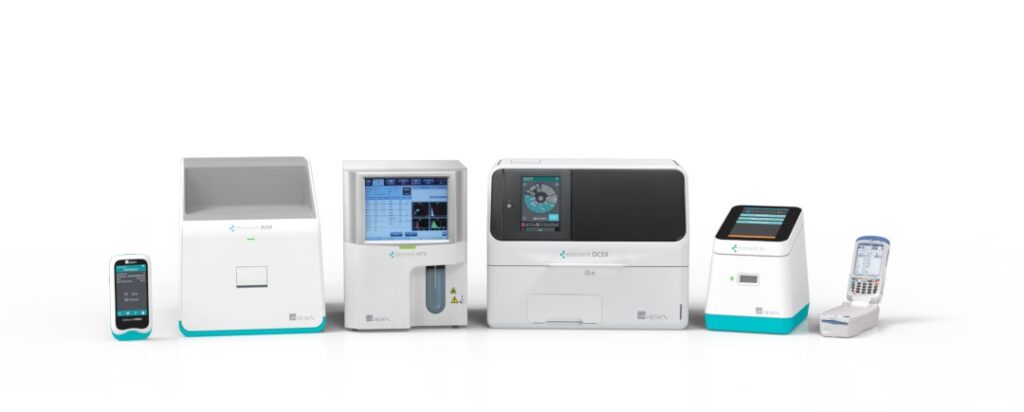
Most toxin ingestions are diagnosed based off history and clinical signs. Lab equipment is essential to understand the complete status of these patients, however.
A complete lab setup should be comprehensive enough to rapidly provide us with all necessary parameters for the veterinarian to make a diagnosis and treatment plan. Diagnostic testing can guide us and answer questions such as what we need to be supplementing versus what does the patient have too much of. It can let us know the efficacy of the treatments we have started. Without proper testing we are missing a key piece of the puzzle and missing that puzzle piece
could potentially slow the patient’s recovery.
When you have the equipment and the team (RVTs and other support staff ) to help with these diagnostics, you will have your patients home and enjoying family time in no time.
Conclusion
The holiday season is filled with excitement and activity. Our pets can enjoy this time just as much as we can, but there is more risk to them than other times of the year.
We need to understand the common toxins that are seen (the ones listed in this article do not make a conclusive list), and the processes needed (including diagnostic testing) to help these animals in a timely manner.
Unusual toxins also happen. For those, remember there are resources available that are very helpful. If you have questions regarding a potential toxin you are unsure about, make sure to call the ASPCA Animal Poison Control Line at 1-888-426-4435. This is a very helpful service for both pet owners and veterinary professionals alike. They have certainly helped me many times!
Let’s help our clients keep the holiday season safe and enjoyable for all members of their families!
References:
https://www.merckvetmanual.com/toxicology/food-hazards/
https://www.aspca.org/pet-care/animal-poison-control

